A brief history of the ASSFN and of Stereotactic and Functional Neurosurgery
Meaghan O’Malley
Shabbar F. Danish, MD
Updated June 17, 2024
Officially founded in 1973, the American Society for Stereotactic and Functional Neurosurgery (ASSFN) is a result of the collaborative efforts of decades of thinkers. From the beginning of the twentieth century to today, the leaders in the field of stereotactic and functional neurosurgery have been connected by a common purpose, to improve lives and drive innovation.
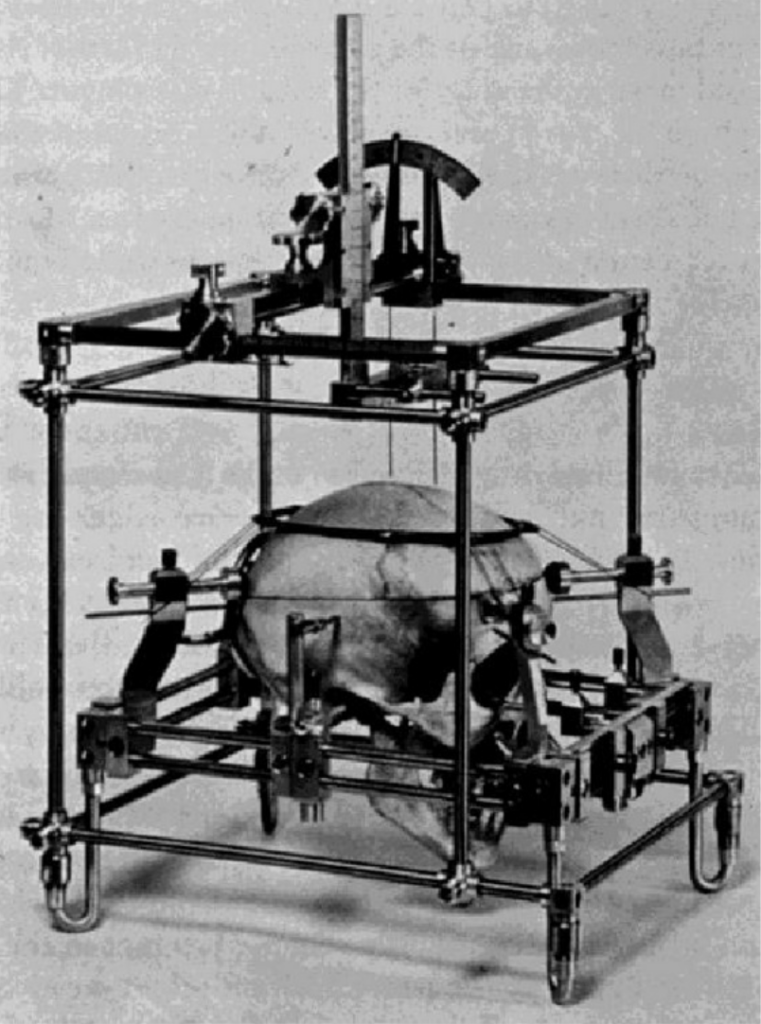
Even before the foundation of a common society for leaders in stereotactic and functional neurosurgery, pioneers in development readily exchanged ideas and built off of each other’s work. Victor Horsley and Robert Henry Clarke’s stereotactic frame ensured accurate access to targeted areas of the brain during surgery on animals.1 The frame used landmarks outside of the skull to pinpoint regions inside the brain.1 Relying on landmarks on the surface of the skull was not accurate enough for human use, due to the variability of human skulls.2 In 1947, Earnest Spiegel and Henry Wycis developed a stereotactic frame for human use using images of the brain taken through pneumoencephalography; these internal landmarks provided the necessary degree of accuracy for further development of functional neurosurgery.1-2 However, this development did not happen overnight. For the next two decades, surgeons worked towards discovering the best possible techniques to alleviate the involuntary movements associated with neurological disorders.
After years of separated but collaborative work among surgeons in this blossoming field, the International Society for Research in Stereoencephalotomy was formed in 1961 to facilitate the exchange of methods and ideas between members of the field.2 In 1973, the name of the foundation was changed to the World Society for Stereotactic and Functional Neurosurgery (WSSFN).2 This update coincided with the establishment of the American Society for Stereotactic and Functional Neurosurgery (ASSFN), as well as the European division (ESSFN).2 The WSSFN has met every four years since 1977.2 The ASSFN and ESSFN also met every four years, but in the period between WSSFN meetings.2 Due to the ever increasing popularity of ASSFN meetings, it was decided in 2003 to start meeting biennially.4 Despite the geographic distinctions between the societies, the attendance at both ASSFN and ESSFN meetings has been truly international, echoing the collaborative beginnings of the field.
Table 1: ASSFN Meetings Since 1980.2,4-6
| Year | Presiding ASSFN President | Meeting Location |
| 1980 | Philip L. Gildenberg | Houston, Texas |
| 1983 | George A. Ojemann | Durham, North Carolina |
| 1987 | Patrick J. Kelly | Montreal, Québec |
| 1991 | Dennis E. Bullard | Pittsburg, Pennsylvania |
| 1995 | Michael L. J. Apuzzo | Los Angeles, California |
| 1999 | Philip L. Gildenberg | Snowbird, Utah |
| 2003 | Douglas Kondziolka | New York, New York |
| 2004 | G. Rees Cosgrove | Cleveland, Ohio |
| 2006 | Andres M. Lonzano | Boston, Massachusetts |
| 2008 | Michael Schulder | Vancouver, British Columbia |
| 2010 | Philip Starr | New York, New York |
| 2012 | Ali R. Rezai | San Francisco, California |
| 2014 | Konstantin Slavin | Washington D.C. |
| 2016 | Aviva Abosch | Chicago, Illinois |
| 2018 | Emad Eskandar | Denver, Colorado |
| 2020 | Robert Gross | Virtual |
| 2022 | Joseph Neimat | Atlanta, Georgia |
| 2024 | Andre Machado | Nashville, Tennessee |
The first ASSFN meeting was held in 1980 in Houston.2 Much of the focus of this meeting centered on the integration of technology into neurosurgery.2 All subsequent ASSFN meetings have demonstrated a pointed interest in the advancement of technology used in surgery, whether that be for imaging or operation.
L-dopa, a medication used to treat Parkinson’s, was introduced during the 1960s and 70s and resulted in a decreased interest in stereotactic neurosurgery.1-2 Interest in stereotactic functional neurosurgery was revived in the late 80s and early 90s by Finish surgeon Lauri Laitinen.1 Drawing from Lars Leksell’s interest in posteroventral pallidotomy as a treatment for Parkinson’s, Laitinen found an effective treatment to both symptoms of Parkinson’s and side effects of L-Dopa.1 Laitinen also helped usher in a new age of image-guided stereotactic surgery as he was one of the first to use stereotactic MRI in surgery.1 Laitinen presented his findings at the 1991 ASSFN meeting in Pittsburgh.2
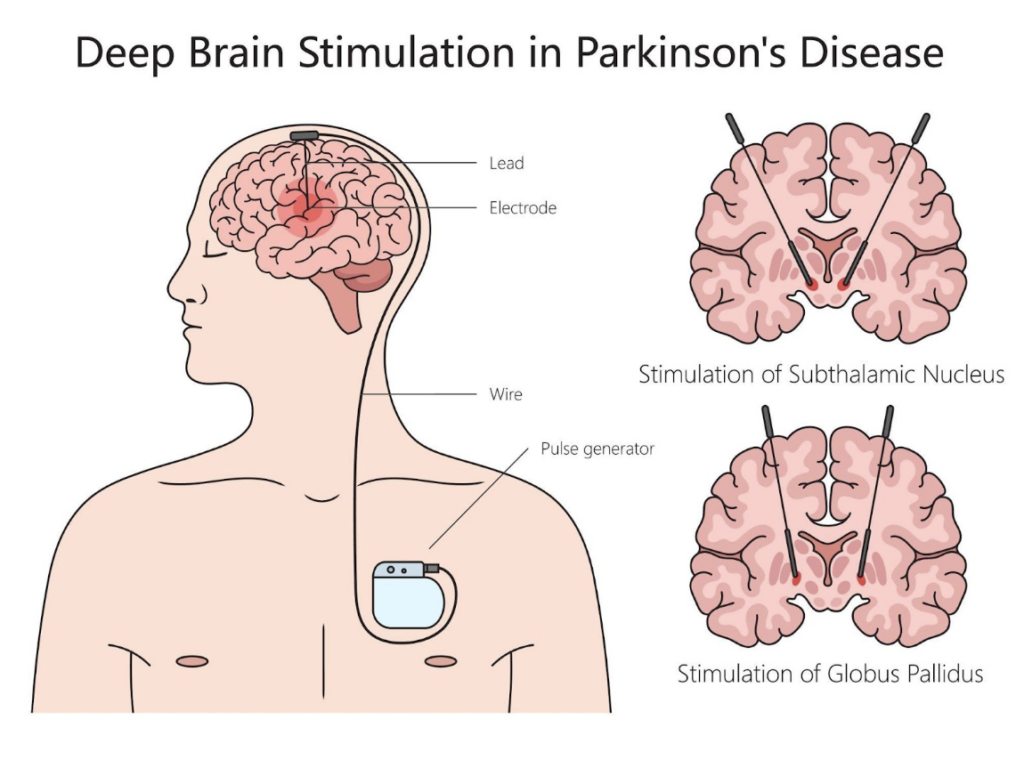
Development in the field of neurosurgery has led to advancements in methodology and technology for treatment in various subspecialties including epilepsy, pain, and movement disorders. Today, the most common treatment for various movement disorders, especially Parkinson’s disease, is deep brain stimulation (DBS).1 DBS has been continually developed since the 1950s when it was intended for treatment of chronic pain.1 Natalia Petrovna Bechtereva was the first to use DBS as a treatment for movement disorders.1 Development of this treatment has been ongoing since its impetus, and it has been a topic of discussion at almost every ASSFN meeting since 1980.2 The persistence of the topic of DBS through the history of ASSFN exemplifies the society’s dedication to innovation in order to realize the full potential of functional neurosurgery.

DBS is also used in neuromodulation-based treatment of epilepsy.8 Neuromodulation-based epilepsy treatments use implanted devices to administer electrical stimulation to nerves in the brain.8 While DBS administers constant stimulation, responsive neurostimulation (RNS) reacts to signals in the brain indicating a seizure and stimulates the cortex as a result.8 Both examples of the use of functional neurosurgery in the treatment of epilepsy result in a greatly improved quality of life despite employing different methods to control seizures. In neurosurgery, the treatment of epilepsy is a highly personalized procedure. An electroencephalogram (EEG) is often used to uncover where in the brain the seizure originates.8 If initial EEG results are unclear an intracranial EEG can be used to detect signals from deeper areas of the brain, as well as deliver stimulation to induce seizures and map cortical function.8 MRI is used alongside an EEG to uncover epileptogenic lesions and other malformations in the brain.8
Neuromodulation is also used in the spine for treatment of chronic pain through spinal cord stimulation.8 Leads are placed at certain points on the spine based on the location of the pain and connect to an implanted device which generates a pulse.8 This method was proven more effective than both repeat surgery and nonoperative treatment of pain.8 Often, surgery can be the best option for those suffering from pain that is unresponsive to medication.8 Surgery can also be used to facilitate medication such as through the implantation of intrathecal pain pumps which administer low doses of painkillers with more accuracy and fewer side effects than standard medication.8
One fairly new addition to the field of neurosurgery is stereotactic radiosurgery (SRS). Originated by Lars Leksell in 1968 with the creation of the Gamma Knife, it was not until the mid-1990s that SRS became cemented in the arsenal of ablative treatment options.2,10 SRS has become a highly valuable ablation option for lesions, chronic pain, epilepsy, and movement disorders, among other diseases.2 MRI and CT images are used to establish the target of surgery while a fiducial reference box attached to the patient’s head frame provides coordinates to ensure proper positioning of the brain.11 During the procedure, many precise beams of radiation are sent through the brain toward the surgical target.11 Due to the precision of the beams, the surrounding tissue is unharmed but the lesion is destroyed at the focal point of the rays.11
A similar ablation option to SRS is radiofrequency thermaoablation (RF). Both options are more established treatment options and have been proven both effective and safe through thorough use in the field, and RF is the most commonly used ablation technique.1, 13 RF involves an intracranial electrode which generates heat at the tip of the device.13 The tip of the electrode heats up the surrounding tissue and creates a heat lesions at the desired target.13 One drawback of RF is that although it is minimally invasive it cannot be used to treat larger areas due to the heat lesion made.13

Similarly to RF, laser interstitial thermal therapy (LITT) is a minimally invasive lesioning technique. LITT destroys abnormal cells using laser light transmitted via flexible fiberoptic wires.13 This treatment offers more flexibility than RF as modification to the laser probe can produce different shaped lesions along the path of the wires.13 This ablation technique has been used since the 1970s for brain tumors, and is increasing in popularity as technological advancements improve accuracy.13 Additionally, LITT is used in treatment of chronic pain, movement disorders, and increasingly, epilepsy.13
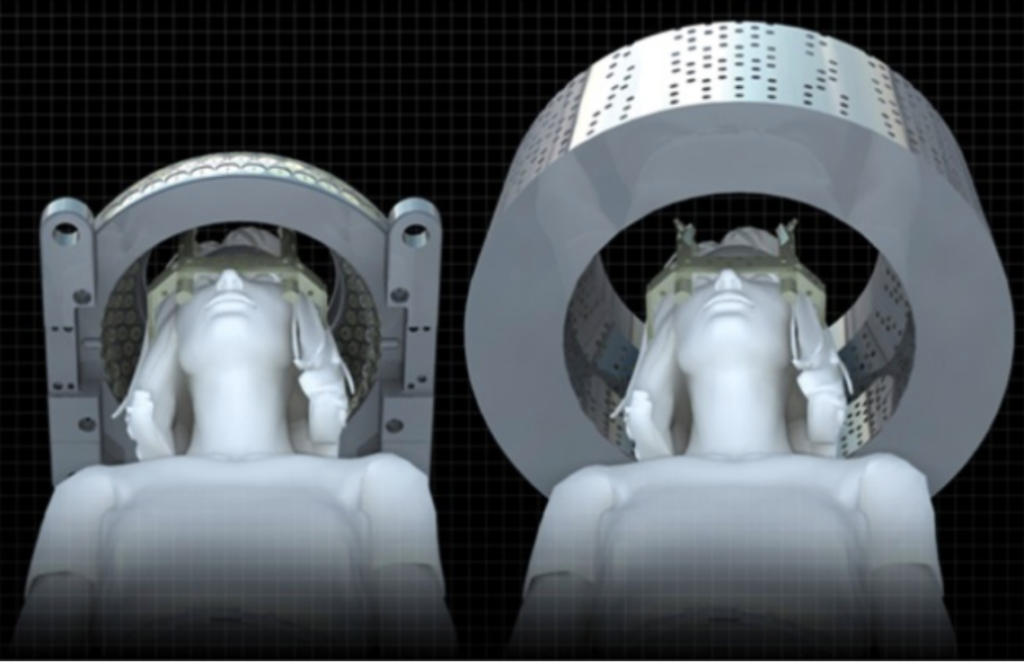
Magnetic resonance-guided focused ultrasound (MRgFUS) is a very recent and highly valuable addition to the world of neurosurgery. Scientists first began studying ultrasound properties in the 1920s, but it was not until the 1980s that ultrasound energy was used in brain tumor ablation.15 Today, MRgFUS uses high intensity focused ultrasound (HIFU) beams emitted from a hemisphere of transducers.13 Similar to SRS, ablation only occurs at the intersection point of these beams while the rest of the brain is left unaffected.13, 15 MRgFUS allows for real time monitoring during the procedure allowing for mid-surgery corrections.15 Advancement in this technique is exciting as MRgFUS is entirely non-invasive, requires almost no hospitalization, and has resulted in very few complications.13, 15

One very interesting development in the space of functional neurosurgery for rehabilitation is Brain-machine interface (BMI). The system uses recordings of brain activity captured by MRI or EEG in order to use signals in the brain to control an external device to facilitate movement such as a prosthetic, frame, or exoskeleton.17 In order to control the external device, users practice motor imagery which involves imagining doing a certain task.17 Motor imagery results in almost the exact same brain activity as actually performing the given task does.17 Development in this treatment is a vital point in rehabilitation for those experiencing paralysis, amputations, stroke recovery, among other problems affecting motor function.17
It must be acknowledged that Stereotactic and Functional Neurosurgery is a constantly evolving subspecialty. There are several aspects of this field including diagnostic and therapeutic tools that go beyond the scope of the introductory content. And just as the field evolves, the Society continues to adapt in order to meet the needs of the field and the patients that require our care.
The history of the American Society for Stereotactic and Functional Neurosurgery offers a glance at decades of innovation and collaboration driven by the common goal of making a positive impact on the lives of others. Development in this field has depended on discovery, rediscovery of abandoned ideas, and continued development of familiar practices. Since 1973, the American Society for Stereotactic and Functional Neurosurgery has provided a point of connection for members to exchange ideas and create connections in order to reach the full potential of functional neurosurgery.
References
- Krauss J, Hariz M, Blomstedt P, et al. A short history of movement disorders.
- Gildenberg P. History of the American society for stereotactic and functional neurosurgery. Meet Am Soc Stereotact Funct Neurosurg. 1999;72: 77-81. 10.1159/000029703
- Grunert P. From the idea to its realization: the evolution of minimally invasive techniques in neurosurgery. Minim Invasive Surg. 2013;2013:171369. doi:10.1155/2013/171369
- Rees Cosgrove G. Stereotactic and Functional Neurosurgery News: Spring 2004. assfn.org. March 12, 2024. Accessed June 7, 2024. Link.
- Gildenberg PL, Krauss LK. Section 1 History of Stereotactic Surgery. In: Lozano AM, Gildenberg PL, Tasker RR, eds. Textbook of Stereotactic and Functional Neurosurgery. Vol 1. 2nd ed. Springer-Verlag; 2009:3-44.
- Slavin KV. Perspectives on the History of the Neuromodulations Societies: Societies for Stereotactic and Functional Neurosurgery. In: Neuromodulation : Comprehensive Textbook of Principles, Technologies, and Therapies. Vol 1. 2nd ed. Academic Press; 2018:3-7.
- Alexander_P. Deep brain stimulation structure parkinson disease stock vector (royalty free) 2425018933. Shutterstock. February 13, 2024. Accessed June 17, 2024. Link
- Chen W, Tariq F, Ashraf K, et al. Role of Functional neurosurgery in Improving Patient Outcomes in Epilepsy, Movement Disorders, and Chronic Pain. Mo Med. 2024;121(2):149-155.
- Larkin M, Meyer RM, Szuflita NS, Severson MA, Levine ZT. Post-Traumatic, Drug-Resistant Epilepsy and Review of Seizure Control Outcomes from Blinded, Randomized Controlled Trials of Brain Stimulation Treatments for Drug-Resistant Epilepsy. Cureus. 2016;8(8):e744. Published 2016 Aug 22. doi:10.7759/cureus.744
- Apuzzo M. A fantastic voyage: a personal perspective on involvement in the development of modern stereotactic and functional neurosurgery (1974-2004). Neurosurgery. 2005; Volume 56 (5): 1115-1131. 10.1227/01.NEU.0000157959.12881.D4
- Hynes PR, Das JM. Stereotactic Radiosurgery (SRS) and Stereotactic Body Radiotherapy (SBRT) Updated 2023 Jul 25. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Link
- Nakazawa H, Tsugawa T, Mori Y, et al. Effective usage of a clearance check to avoid a collision in Gamma Knife Perfexion radiosurgery with the Leksell skull frame. J Radiat Res. 2014;55(6):1192-1198. doi:10.1093/jrr/rru057
- Franzini A., Moosa S., Servello D., et al.. Ablative brain surgery: an overview. International Journal of Hyperthermia. 2019; 6(2), 64–80. Link
- Healthy Definition. Step by step visualase MRI-guided laser stock photo 2429954817. Shutterstock. February 25, 2024. Accessed June 17, 2024. Link
- Mauri G, Nicosia L, Xu Z, et al. Focused ultrasound: tumour ablation and its potential to enhance immunological therapy to cancer. Br J Radiol. 2018;91(1083):20170641. doi:10.1259/bjr.20170641
- Jung NY, Chang JW. Magnetic Resonance-Guided Focused Ultrasound in Neurosurgery: Taking Lessons from the Past to Inform the Future. J Korean Med Sci. 2018;33(44):e279. Published 2018 Oct 4. doi:10.3346/jkms.2018.33.e279
- Ferrero, L., Soriano-Segura, P., Navarro, J. et al. Brain–machine interface based on deep learning to control asynchronously a lower-limb robotic exoskeleton: a case-of-study. J NeuroEngineering Rehabil 21, 48 (2024). Link